Harm reduction has been a hot button political issue lately with lots of misinformation being spread for political and monetary gain. In this article, we will discuss the harm reduction strategies being implemented at Homes First shelters and housing programs to help keep our residents and neighbours safe as well as debunk some common myths about harm reduction.

What is harm reduction?
Harm reduction is an evidence-based approach to reducing individual and community harm from a risky activity. It recognizes and accepts that some activities are risky but the chance of harm can be reduced by implementing certain safety strategies.
A great example is driving a car. Cars are dangerous and kill over 1,500 people a year in Canada, but people are still going to drive cars regardless of the danger posed and this is largely accepted. To help keep ourselves and others as safe as possible, society has implemented safety measures such as seatbelts, airbags, backup cameras, speed limits, traffic lights, etc., to reduce the chance of an accident and harm to those involved in an accident. Nearly all agree that these strategies are logical and research shows that they’re also effective.
Harm reduction takes the same approach for drugs. History has shown that people are going to use drugs whether they’re legal or illegal or could cause them harm. Alcohol is a good example. Alcohol prohibition failed to stop alcohol consumption, so society instead chose to try and reduce the harm caused by it by implementing age restrictions for purchases, drunk driving laws, quality controls on production, labelling the amount of alcohol by volume, etc. Again, these are logical and effective strategies that reduce the chance of harm.
Harm reduction takes a non-judgmental approach to drug use and uses logical strategies supported by decades of research to reduce the amount of harm that comes to people who use drugs and the communities that they live in. Furthermore, harm reduction strategies are cost-effective and save Canadian taxpayers money by preventing infections and other healthcare costs (1, 2, 3, 4).
Why do people use drugs?
People use drugs because drugs make them feel good and in most cases the drug use doesn’t negatively affect a person’s life. In some cases, people develop a problematic relationship with drugs in which the person is using them to self-medicate to treat a mental health condition (ex. anxiety disorder, major depressive disorder) and/or trying forget a traumatic experience (ex. sexual assault, childhood abuse). Many people experiencing problematic drug use would like to reduce their drug use or stop using drugs but a lot of times treatment is inaccessible and can take many years and many attempts to be effective so people try to cope the best they can in the moment.
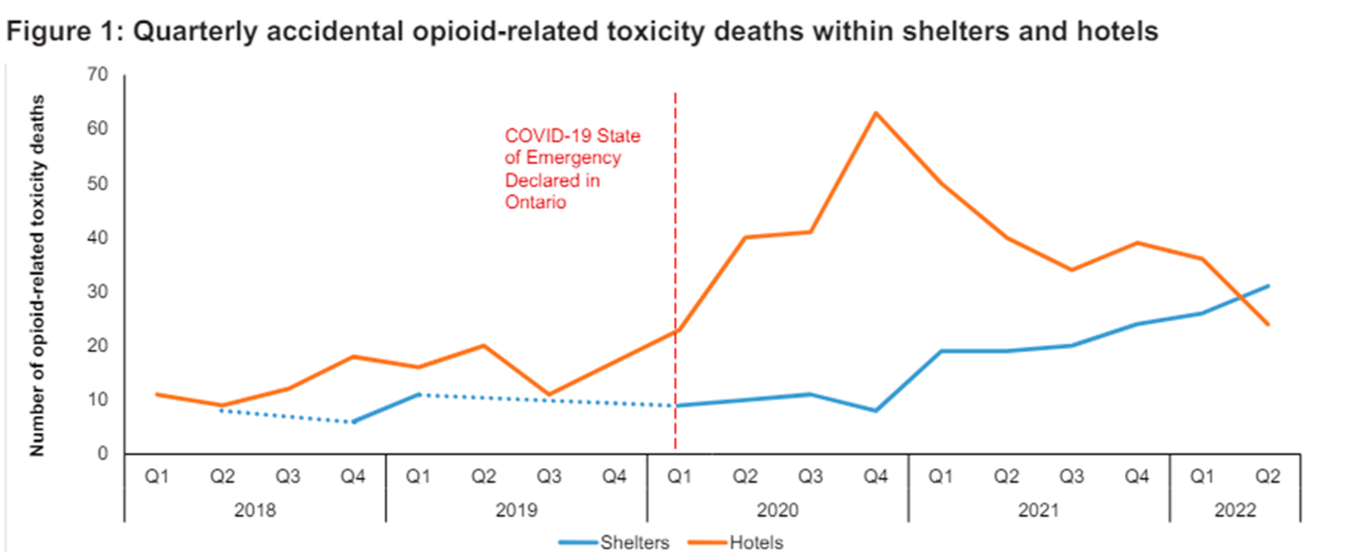
During the COVID-19 pandemic, overdose death in the shelters and shelter hotels increased significantly due to increased variability of the drug supply and people living alone in private rooms (16, 14, Figure 1). All of these issues combined with the general stress of living in a shelter continue to make it difficult for people to regulate their drug use so it’s important that we provide all the harm reduction supports we can to help keep people alive and safe while they try to secure housing and get the treatment supports they desire.
Debunking common myths about harm reduction
There has always been an ideologically driven backlash towards harm reduction since its founding, typically for political gain. Below we’ll debunk a few of the common myths about harm reduction:
Myth 1: If we make drug use safer, more people will use drugs, crime will increase, as will public nuisances associated with drug use.
Fact 1: This is a myth not supported by evidence. On the contrary, decades of evidence shows that harm reduction does not increase community or youth drug use, does not increase crime, and does not increase public nuisance (5, 8, 9). Harm reduction strategies are also cost-effective and save taxpayers money (3, 4, 5).
Myth 2: The ‘tough love’ approach that forces people who use drugs into treatment is the best approach to ending substance use.
Fact 2: A review of the scientific literature shows that most people forced into treatment do not reduce drug use post-treatment, so this strategy doesn’t actually work (10). Additionally, a recent study suggests that mandatory treatment actually increases the chance of overdose once a person leaves treatment (11). This is yet another reason why the United Nations has requested member States to “close compulsory drug detention and rehabilitation centres” (12).
Myth 3: Harm reduction is opposed to abstinence.
Fact 3: Harm reduction supports people making any positive change in their life including–if they want–becoming abstinent from drugs though it does not require it. The reality is that many people figure out over time what drugs they can use and still be able to achieve their goals. Harm reduction is non-judgmental, meets people where they’re at in their life, and provides the support they need to live the life they want whether they’re using drugs or not.
Harm reduction strategies offered at Homes First
Homes First uses internationally recognized harm reduction best practices to improve safety for people who use drugs in our programs. Residents have 24/7 access to clean syringes, pipes, and sharp disposal bins—so needles and pipes are safely disposed and no need to share supplies which prevents the spread of HIV and hepatitis C—as well as naloxone so residents can respond immediately to overdoses both on and off-site.
Homes First also trains its staff on substance use and harm reduction strategies to ensure that staff are equipped with the knowledge and skills to support residents who use drugs. A key focus of our staff training is on opioid overdose response as many residents use opioids regularly. Opioid overdoses cause a person to stop breathing which can lead to brain damage and death. We train our staff on naloxone administration–a safe and effective drug that counteracts the effects of opioids–to help get people breathing again. Naloxone takes a few minutes to work so our staff are also trained to use portable oxygen tanks to immediately administer oxygen to a person experiencing an overdose to prevent brain damage and death.
Additionally, we partner with community harm reduction agencies and health organizations who provide additional supports to help keep our residents who use drugs safe and healthy.
For instance, Toronto Public Health operates an overdose prevention site (OPS) at our 545 Lakeshore Blvd West shelter to reduce drug use in the surrounding neighbourhood, reduce drug use in shelter washrooms and showers, and provide a sanitary space for people to inject drugs under supervision so overdoses can be responded to immediately (5). Overdose Prevention Sites also provide people with dignity and help connect them to healthcare, treatment, and social supports in addition to reducing overdose deaths and healthcare costs (4, 5, 6, 7). Our harm reduction partners from Parkdale-Queen West Community Health Centre, The Neighbourhood Group (TNG), South Riverdale Community Health Centre, Street Health, and Sherbourne Health also provide additional supports to residents, educate people who use drugs on best-practices that will help keep them safe, and conduct community clean-ups to improve neighbourhood safety.
Furthermore, our collaboration with Inner City Health Associates (ICHA) provides on-site health and mental health support for clients in shelters and shelter hotels. Many of our sites also have an on-site pharmacy run by TrustCare Pharmacy which makes it easier for people to access all of their medications–including methadone, buprenorphine, and safer supply–to help keep them healthy and prevent harm.
Harm Reduction saves lives!
Overdose deaths increased significantly during the COVID-19 pandemic (14, 15) and the illicit drug supply has become more toxic and unpredictable each year since (16). Harm reduction accepts people for who they are, keeps people who use drugs and the community safe, saves taxpayers money, and helps get people the supports they need to stabilize their lives. We at Homes First are proud to be implementing harm reduction best-practices that keep our residents alive and healthy so they can lead happy and fulfilling lives.
References:
- Tonin FS, Alves da Costa F, Fernandez-Llimos F. Impact of harm minimization interventions on reducing blood-borne infection transmission and some injecting behaviors among people who inject drugs: an overview and evidence gap mapping. Addict Sci Clin Pract. 2024 Feb 4;19(1):9. doi: 10.1186/s13722-024-00439-9. PMID: 38310293; PMCID: PMC10838443.
- Tapper A, Ahern C, Graveline-Long Z, Newberger NG, Hughto JMW. The utilization and delivery of safer smoking practices and services: a narrative synthesis of the literature. Harm Reduct J. 2023 Oct 27;20(1):160. doi: 10.1186/s12954-023-00875-x. PMID: 37891658; PMCID: PMC10612300.
- Nguyen TQ, Weir BW, Des Jarlais DC, Pinkerton SD, Holtgrave DR. Syringe exchange in the United States: a national level economic evaluation of hypothetical increases in investment. AIDS Behav. 2014 Nov;18(11):2144-55. doi: 10.1007/s10461-014-0789-9. PMID: 24824043; PMCID: PMC4211599.
- Andresen MA, Boyd N. A cost-benefit and cost-effectiveness analysis of Vancouver’s supervised injection facility. Int J Drug Policy. 2010 Jan;21(1):70-6. doi: 10.1016/j.drugpo.2009.03.004. Epub 2009 May 6. PMID: 19423324.
- Potier C, Laprévote V, Dubois-Arber F, Cottencin O, Rolland B. Supervised injection services: what has been demonstrated? A systematic literature review. Drug Alcohol Depend. 2014 Dec 1;145:48-68. doi: 10.1016/j.drugalcdep.2014.10.012. Epub 2014 Oct 23. PMID: 25456324.
- Marshall BD, Milloy MJ, Wood E, Montaner JS, Kerr T. Reduction in overdose mortality after the opening of North America’s first medically supervised safer injecting facility: a retrospective population-based study. Lancet. 2011 Apr 23;377(9775):1429-37. doi: 10.1016/S0140-6736(10)62353-7. Epub 2011 Apr 15. PMID: 21497898.
- Rammohan I, Gaines T, Scheim A, Bayoumi A, Werb D. Overdose mortality incidence and supervised consumption services in Toronto, Canada: an ecological study and spatial analysis. Lancet Public Health. 2024 Feb;9(2):e79-e87. doi: 10.1016/S2468-2667(23)00300-6. PMID: 38307685.
- Marx, M.A., Brahmbhatt, H., Beilenson, P. et al. Impact of Needle Exchange Programs on Adolescent Perceptions About Illicit Drug Use. AIDS Behav 5, 379–386 (2001). https://doi.org/10.1023/A:1013195108756
- Marx MA, Crape B, Brookmeyer RS, Junge B, Latkin C, Vlahov D, Strathdee SA. Trends in crime and the introduction of a needle exchange program. Am J Public Health. 2000 Dec;90(12):1933-6. doi: 10.2105/ajph.90.12.1933. PMID: 11111271; PMCID: PMC1446444.
- Werb D, Kamarulzaman A, Meacham MC, Rafful C, Fischer B, Strathdee SA, Wood E. The effectiveness of compulsory drug treatment: A systematic review. Int J Drug Policy. 2016 Feb;28:1-9. doi: 10.1016/j.drugpo.2015.12.005. Epub 2015 Dec 18. PMID: 26790691; PMCID: PMC4752879.
- Rafful C, Orozco R, Rangel G, Davidson P, Werb D, Beletsky L, Strathdee SA. Increased non-fatal overdose risk associated with involuntary drug treatment in a longitudinal study with people who inject drugs. Addiction. 2018 Jun;113(6):1056-1063. doi: 10.1111/add.14159. Epub 2018 Feb 13. PMID: 29333664; PMCID: PMC5938130.
- Joint statement on compulsory drug detention and rehabilitation centres ILO, OHCHR, UNDP, UNESCO, UNFPA, UNHCR, UNICEF, UNODC, UN Women, WFP, WHO and UNAIDS. Geneva: Unitd Nations Office of the High Commissioner for Human Rights; 2012.
- Candian Centre on Housing Rights. A Primer on Financialization of Housing in Canada. https://housingrightscanada.com/a-primer-on-financialization-of-housing-in-canada/.
- Hamzat B, Leece P, McCormack D, Holton A, Dodd Z, Firestone M, Wolfson-Stofko B, Smuts H, Sereda J, Smoke A, Watford J, Watts T, Shearer D, Schneider E, Singh S, Cheng C, Gomes T, on behalf of the Ontario Drug Policy Research Network and Ontario Agency for Health Protection and Promotion (Public Health Ontario). Opioid-related toxicity deaths within Ontario shelters: circumstances of death and prior medication and healthcare use. Toronto, ON: Ontario Drug Policy Research Network; 2024.
- Public Health Ontario. Interactive Opioid Tool: Opioid-related morbidity and mortality in Ontario. https://www.publichealthontario.ca/en/Data-and-Analysis/Substance-Use/Interactive-Opioid-Tool
- Thompson H, McDonald K, Maghsoudi N, Werb D. Toronto’s increasingly unpredictable and toxic unregulated opioid supply. Results from samples checked by Toronto’s Drug Checking Service: January 1 – December 31, 2022. Toronto: Centre on Drug Policy Evaluation. April 30, 2023.
This blogpost was written by Dr. Brett Wolfson-Stofko, Manager of Harm Reduction at Homes First and edited by Michael Potvin, PhD Candidate and Director of Client Services at Homes First.


